How Often Should You Change Your Catheter? A Guide to Catheter Replacement and Supply Coverage
Managing a catheter can be challenging, but knowing how often to change it and what supplies are covered by insurance can make the process easier. This guide will walk you through the recommended replacement schedules for different types of catheters and provide information on Medicare coverage for catheter supplies.
Types of Catheters and Replacement Schedules:
There are several types of catheters, each designed for specific needs and with their own recommended replacement schedule:
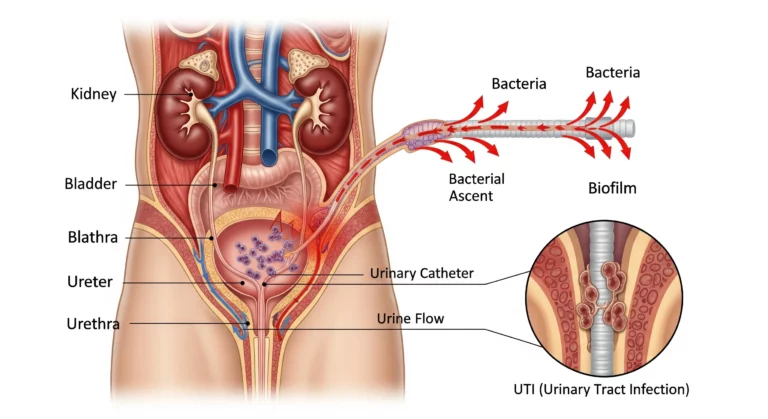
- Indwelling/Foley Catheters: These catheters reside within the bladder and are typically held in place by a small balloon. They require regular changes to minimize the risk of infection and other complications. Generally, indwelling catheters should be changed every 4-6 weeks, or as directed by your healthcare provider.
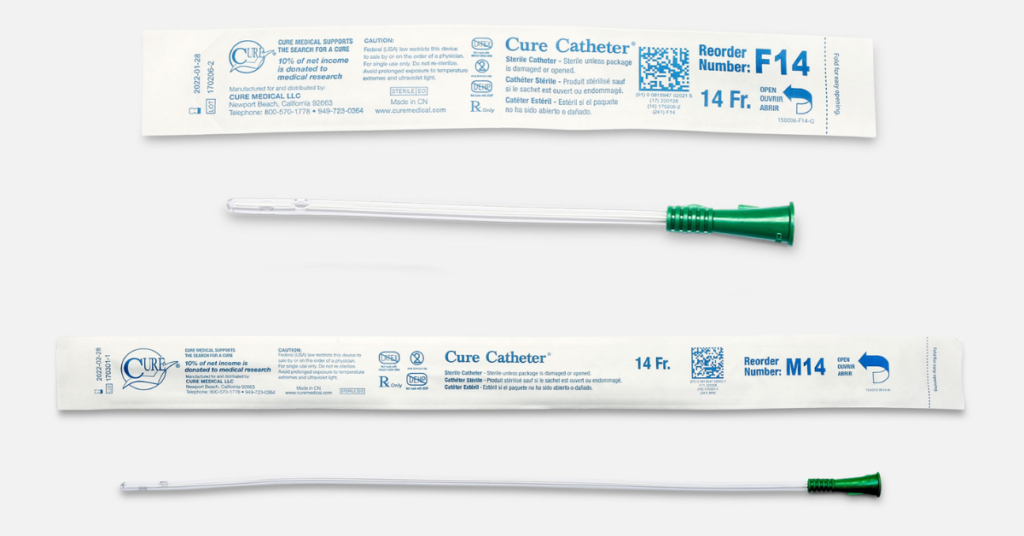
- Intermittent Catheters (Straight/Coudé Tip): These catheters are inserted and removed each time the bladder needs to be emptied. They are available in straight and coudé (curved) tip variations. While the catheter itself is single-use, the frequency of use depends on individual needs. Supplies, like lubricant and wipes, are important.
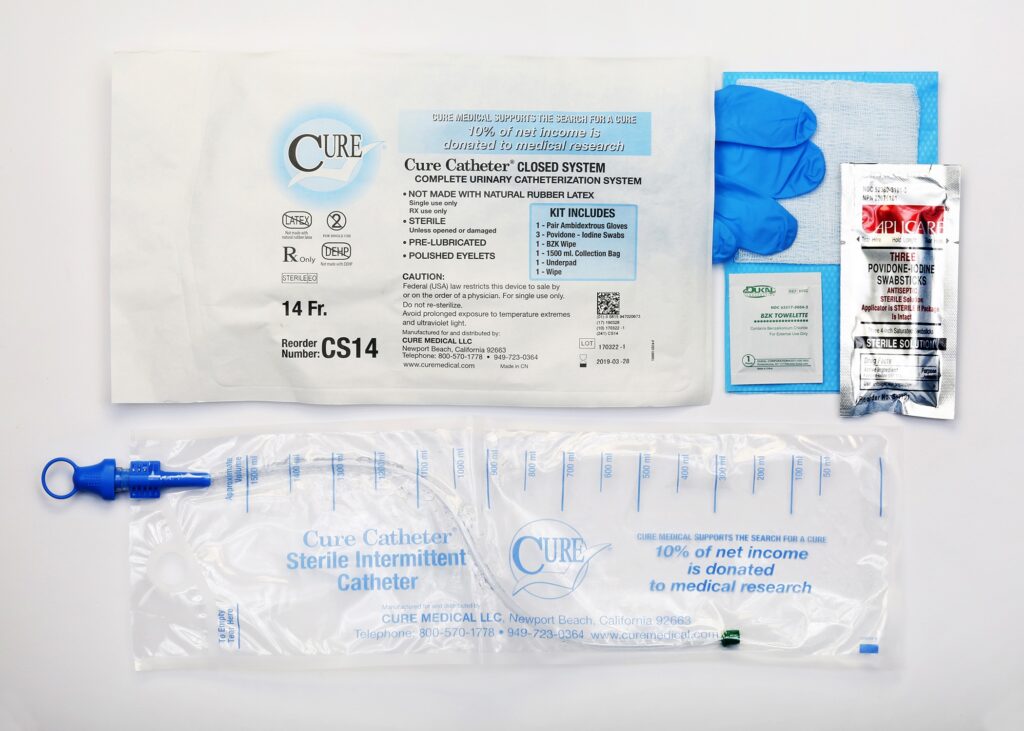
- Closed System Catheters: These are a type of intermittent catheter that includes a collection bag, creating a closed system to reduce the risk of urinary tract infections. They are also single-use.
- External Catheters: These catheters are worn externally and are a non-invasive option for managing urinary incontinence. They should be changed daily to maintain hygiene and prevent skin irritation. There are two main types.
- Male External Catheters (Condom Catheters): These are applied to the penis like a condom and connected to a drainage bag. They come in various sizes and styles to ensure a proper fit.
- Female External Catheters: (Urinary Collection Devices): These typically consist of a form-fitting device that adheres around the urethra and a collection bag. They offer a discreet and comfortable alternative to indwelling catheters for women.
Medicare Coverage for Catheter Supplies
Medicare Part B covers many catheter supplies when prescribed by a doctor for a medically necessary condition. However, there are limitations on the quantity of supplies that can be covered within a specific timeframe. It’s crucial to understand these limitations to avoid unexpected out-of-pocket costs. The following table provides a general overview based on CMS.gov information. It is best to consult with your provider and insurance company to ensure up-to-date and specific coverage for your situation.
Supply | Medicare Coverage Guidelines (General) | Notes |
Indwelling Catheters | Usually one catheter and insertion supplies per month. | Coverage may vary depending on individual circumstances and medical necessity. |
Intermittent Catheters | Up to 200 catheters per month (varies by type and individual need). | Coverage for lubricant, wipes, and other related supplies is also available. Closed system catheters may have different coverage guidelines. |
Male External Catheters | Generally, no more than 35 per month. More may be covered if your doctor provides a medical reason. | Specialty catheters (like those that inflate or have a special design) require your doctor to explain why you need that specific type. |
Female External Catheters | No more than one metal cup per week and one pouch per day. | |
Collection Bags (for indwelling) | Varies, typically based on need. | Consult with your provider and insurance. |
Medicare Advantage, Medicaid and Commercial plans may also cover catheters and related supplies. What is covered and how often may vary from plan to plan. Our urology team can try to help answer questions surrounding policies specific to non-Medicare plans. You can give our team a call at 866.864.6332.